Lead image from iStock
By Jena Lynde-Smith
In the neonatal intensive care unit (NICU), every second counts. For babies fighting for their lives, traditional wired sensors play a crucial role in monitoring vital signs like blood oxygen levels and heart rate. However, these sensors come with limitations, from causing false alarms and disturbing fragile infant skin to impeding parental bonding.
Jim Green, a Carleton University Systems and Computer Engineering professor is collaborating with the CHEO, a pediatric healthcare and research centre in Ottawa, to pioneer a new approach to patient monitoring using non-contact sensors that monitor vital signs with minimal disruption to the baby’s environment.
“Two of my own children were treated in the NICU,” says Green. “I have always sought to apply engineering to solve problems in the biomedical field, but working with the NICU is especially important to me.”

Non-Contact Patient Monitoring
The NICU is a busy and loud environment, with constant activity and alerts. Of the many alarms heard, around 50 per cent are false. These false alarms are often caused by motion artifacts, which occur when a baby’s movement disrupts the sensor readings. Sensor displacement and environmental interference from other medical devices also contribute to false alarms – as well as changes in skin such as sweat and temperature.
To help address this issue, Green has created non-contact, unobtrusive sensors that don’t require direct connection to an infant’s skin.
“The first goal was to reduce false alarms, which not only create a stressful environment for families but can lead to clinician fatigue and, dangerously, the potential to miss a true alarm,” says Green.

Jim Green, Carleton Systems and Computer Engineering professor
He and his team of a dozen graduate students explored two new types of neonatal sensors: a pressure-sensitive mat that goes under the infant and a video camera that is positioned above the baby’s bed. The pressure-sensitive mat, which resembles a simple black bed sheet, detects time-varying contact pressure, which, when processed using machine learning, can estimate respiration rate and detect what certain movements mean.
“The mat is actually so sensitive that as the baby breathes, even though it’s just a slight bounce on the mattress from the chest rising and falling, we can extract the respiration signal from all the noise and get an estimate of respiration rate,” Green explains.

Green and his team explored two new types of neonatal sensors: a pressure-sensitive mat that goes under the infant and a video sensor that is positioned above
The video sensor provides both color (RGB) and depth (D) footage using an Intel RealSense camera. This technology, which has advanced significantly since the days of the Microsoft Kinect, is now consumer-grade, offering improved accuracy at a lower cost. By analyzing the changes in the red channel of the baby’s face, the camera can estimate heart rate.
“These non-contact sensors enhance the capabilities of traditional wired sensors by adding layers of context,” Green says.
“For example, the pressure-sensitive mat can tell us that the baby isn’t even in their bed, and the video sensor can let us know that a sensor is disconnected due to bathing or feeding.”

Advancing the NICU with AI
One of the most promising aspects of Green’s research is the integration of artificial intelligence (AI) to interpret sensor data. By using machine learning algorithms, his team analyzes the context of the baby’s environment to differentiate between interventions, such as feeding, bathing, or diaper changes.
“This information could change how clinicians interpret alarms and care for their tiny patients,” says Green.
To train a machine learning system, Green and his students manually observed patients in CHEO’s NICU that were using the pressure-sensitive mat and video sensor. They worked in collaboration with Dr. JoAnn Harrold, now-retired nurse Cheryl Aubertin, and retired Director of Clinical Engineering, Kim Greenwood.
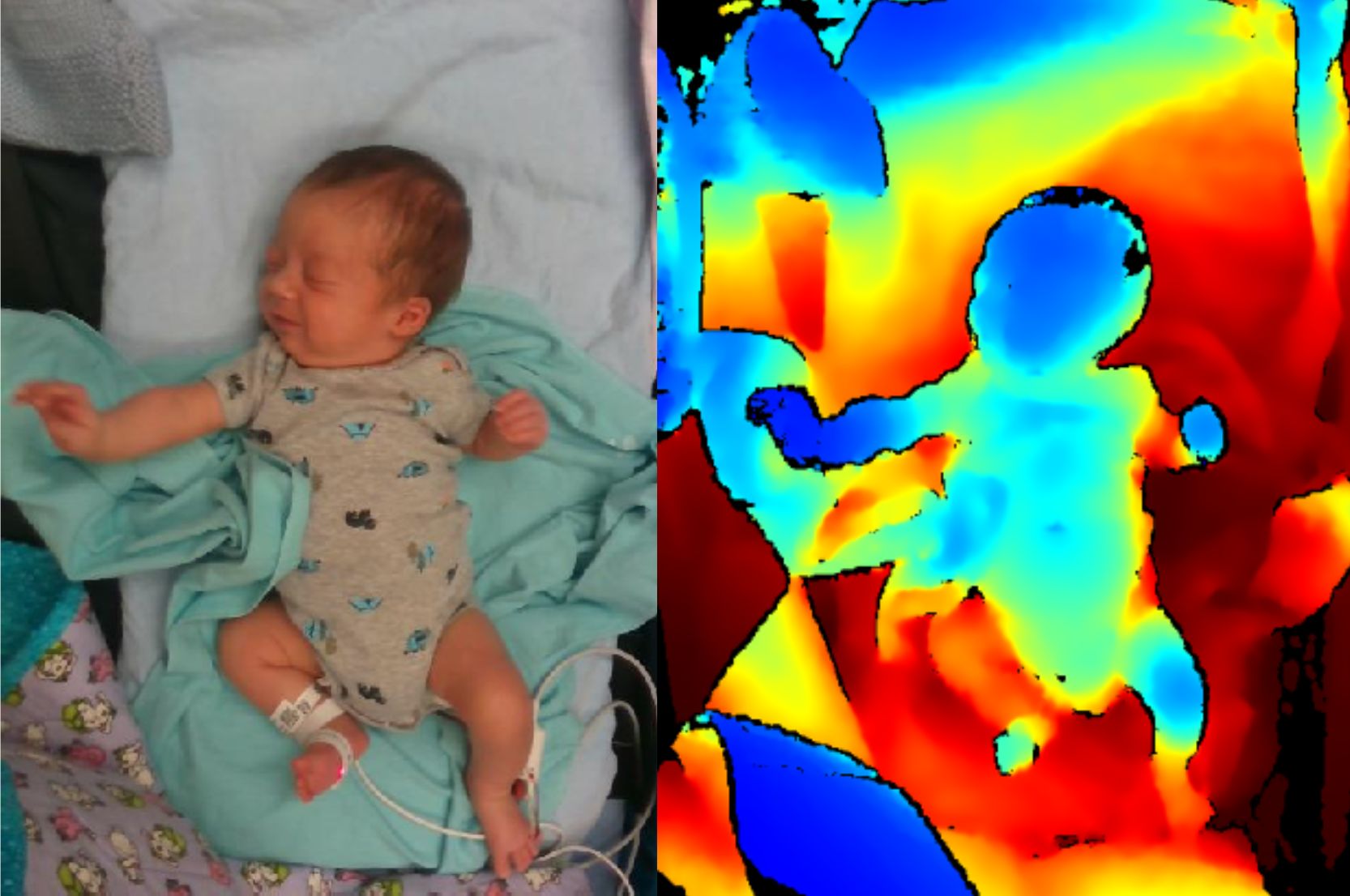
The video sensor provides both color (RGB) and depth (D) footage that can detect a baby’s heart rate
Green’s team observed 32 children from vulnerable premature infants to nearly ready-for-discharge babies. Spending an average of four hours collecting data on each patient, they often conducted their studies in the middle of the night to avoid disrupting parent visits. Using an application they developed for an iPad, they manually inputted each event of clinical significance such as sneezes and coughs, alarms and routine care events like diaper changes.
“We wanted to capture all the events of clinical significance in real time to align it with the sensor data, so that later we can detect things like coughs and sneezes just from specific spikes on the pressure sensitive mat,” Green explains.

Toyin Adams, fourth-year Carleton engineering student
Toyin Adams, a fourth-year Software Engineering student supervised by Green, is taking the integration of AI in the NICU one step further. With the information collected from the non-contact sensors, she is using open-source large language models – advanced computer programs that understand and generate human language – to develop a system that can send automated text messages to parents, clinicians, and researchers.
Each message is tailored based on the audience needs. For example, a parent may receive a concise update on their baby’s condition, while a clinician would receive a more detailed report for handover rounds.
“The potential benefits of automated message generation from non-contact sensor data are significant,” says Adams. “In critical environments like the NICU, where quick decisions are crucial, such summaries could be a game-changer for clinicians.”

Reducing Family Stress
While his current work is looking at how wired and non-contact sensors may be able to work together, Green sees a world where wireless sensors could become the standard.
“Not only could these non-contact sensors improve infant care in the NICU, but they open up the opportunity for more parental bonding where parents may be able to scoop up their baby without being tangled with wires,” Green says.
By reducing the reliance on wired sensors and introducing non-contact monitoring, this technology could not only improve care within the NICU but also extend to home use.
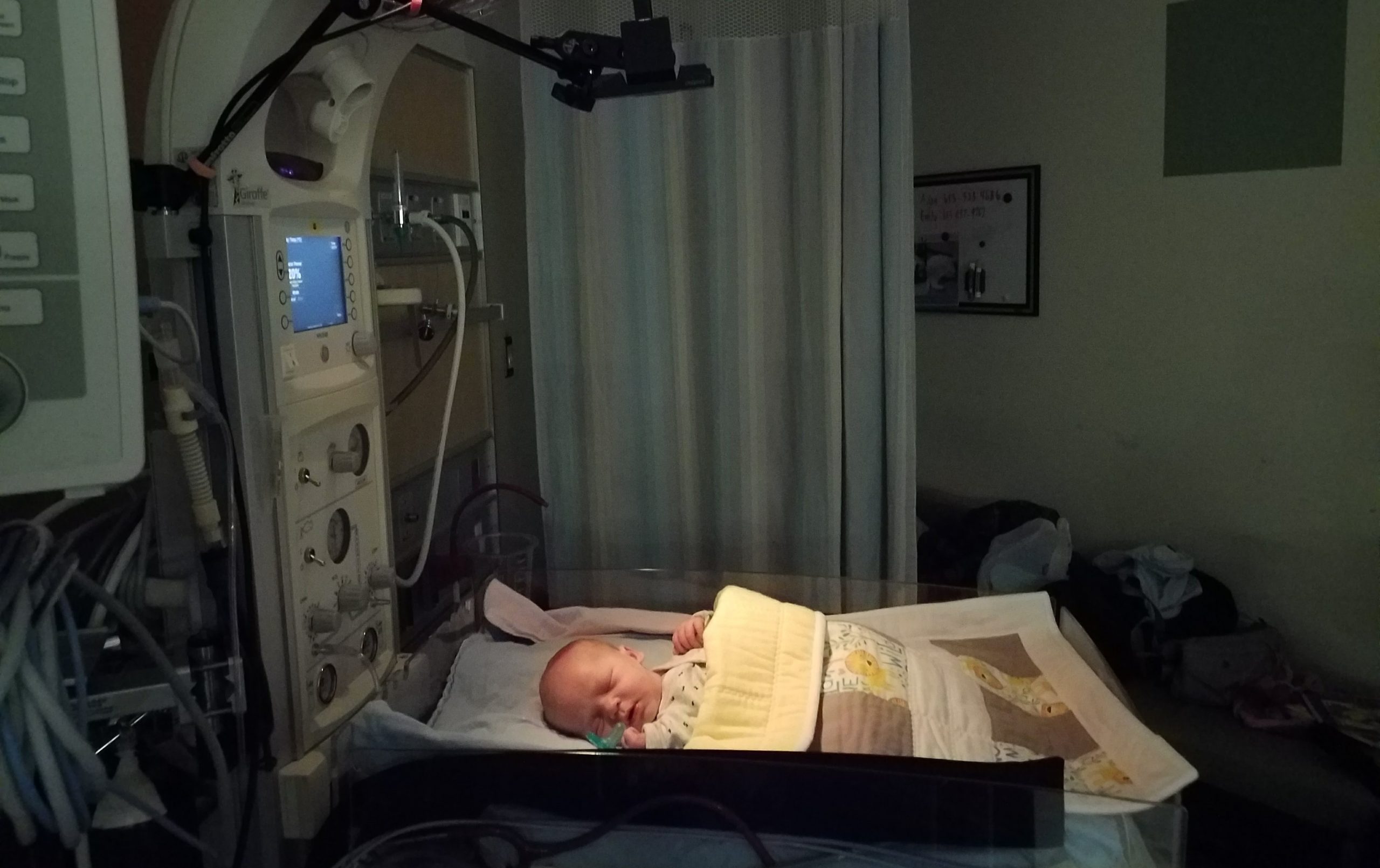
Green’s team observed 32 babies in CHEO’s NICU, often through the night to avoid disrupting parental bonding
“Imagine a scenario where a premature baby has been discharged but still requires monitoring. Instead of being tethered to wired sensors, the baby could be at home, comfortably nestled in a crib equipped with non-contact sensors,” explains Green.
“We want to minimize the impact and stress on families.”
Green has experienced this stress first-hand.
“I know how overwhelming it can be to have a baby in the NICU,” he says.” My personal experiences have motivated me to find ways to make this challenging time a little easier for other families.”

Full width photos from iStock
Wednesday, June 5, 2024 in Engineering, Health, Partnerships
Share: Twitter, Facebook



