By Joseph Mathieu
Photos by Brenna Mackay
You don’t have to be a donor or a doctor to know that Canada regularly faces an unstable blood supply.
Wholly dependent on individuals who can only donate every two to three months, the system is a tenuous one—always needing more donations and regularly affected by outside forces, from pandemics to bad driving weather. Our national blood supply is always in need of a shot in the arm.
Getting and keeping platelets—the blood cells that bind together when they recognize damaged blood vessels—is even more difficult. They only last a week, kept at room temperature and with continuous agitation. They are highly vulnerable to bacterial contamination. And there’s always the chance that a patient’s body will not accept someone else’s platelets.

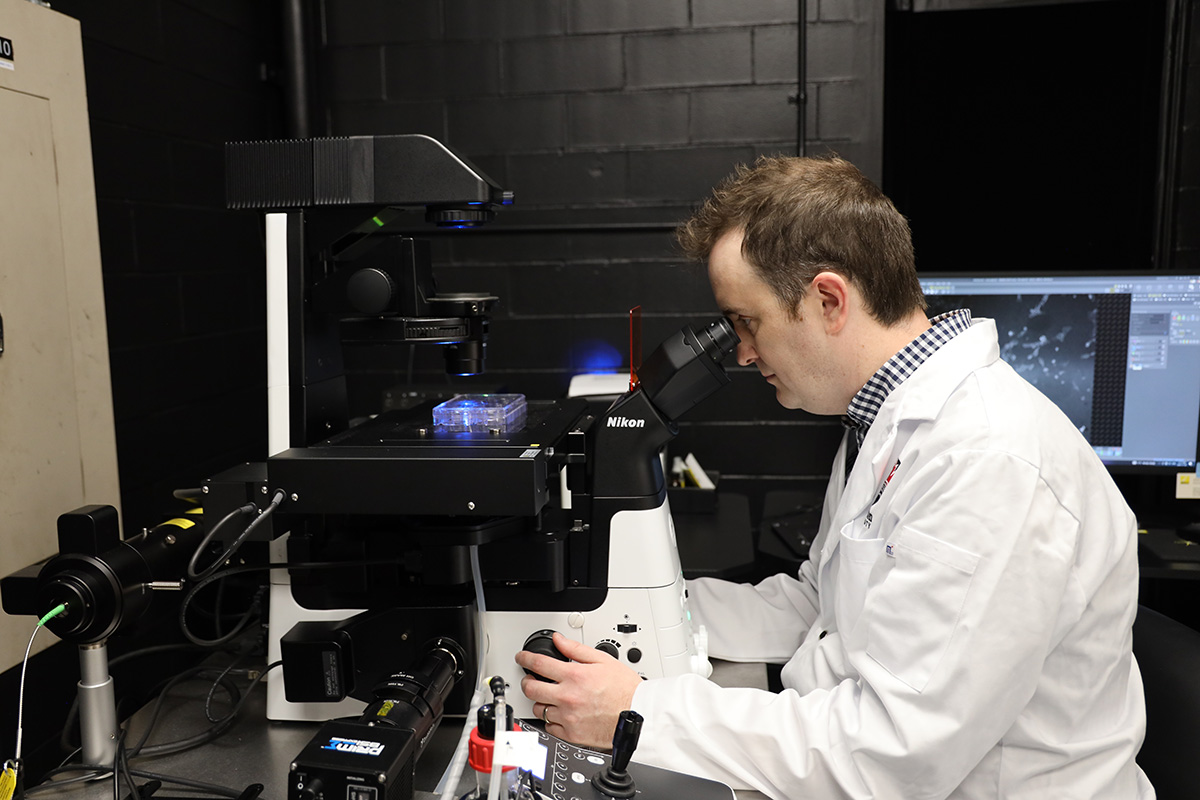
Mechanical and Aerospace Engineering Assistant Professor Andrew Harris
According to Canadian Blood Services, they are the most in-demand blood product in our healthcare system and also the most often discarded.
“Can we, therefore, just make platelets without a donor?” asks Andrew Harris, an assistant professor of Mechanical and Aerospace Engineering at Carleton University.
“Not yet.”
Platelet Challenges and Synthetic Solutions
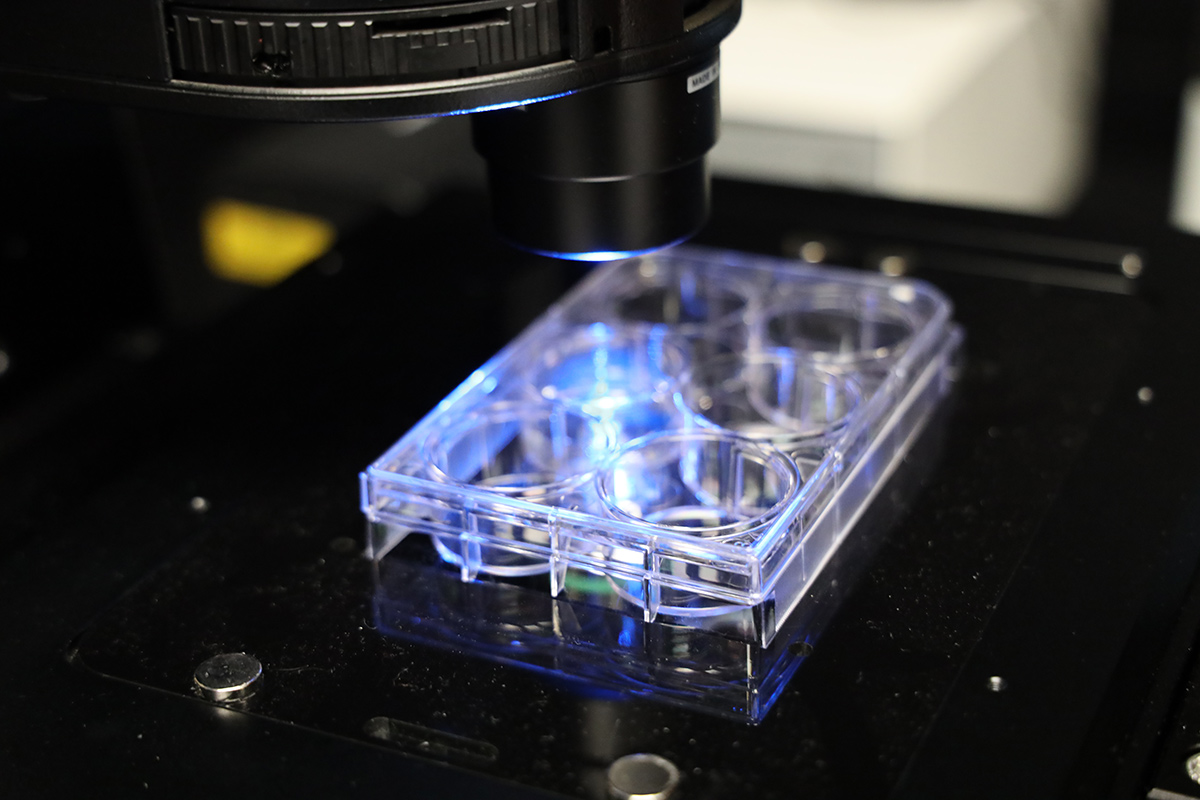
Thanks to stem cells, it is possible to generate platelet-producing cells in a lab, but current methods do not produce enough platelets to achieve an effective transfusion. Harris believes the key to a viable, plentiful source of synthetic platelets is in understanding these cells from a materials science and engineering perspective.
“Cells that produce platelets need to basically contract and then pinch off a piece of themselves into the bloodstream. It involves generation of force, a change in cell shape and a protrusion,” says Harris. “That is a very mechanical process.”
A Banting Research Foundation’s Discovery Award for innovative health and biomedical research projects will allow Harris to investigate how platelet-producing cells generate these forces, what the material characteristics of these cells are and how changes to these characteristics can lead to disease.
“What we’re hoping to do is gain new insights into how platelets are produced, and maybe develop new ways that we can produce platelets to reduce the dependence on donor-source platelets for transfusions,” he says in his 2023 Banting Discovery Awardee video.
During his Master of Physics degree at the University of Leeds, Harris became interested in using physics tools to answer biological questions: How do cells organize to create organs? Why do some tissues fail as we age? How do stem cells decide which will remain stem cells and which will become specialized cells—in blood, brain or bone?
His PhD in Engineering from University College London took this work further to understand how the physical properties of tissues affect their physiological behaviour. Today, Harris looks into designing cells and tissues for a variety of systems including the kidney, gut, skin and blood. Research between cell biology and the mechanical properties of tissues is the core of his Cell and Tissue Engineering Laboratory (CTELab) at Carleton.
CTELab and Future Applications
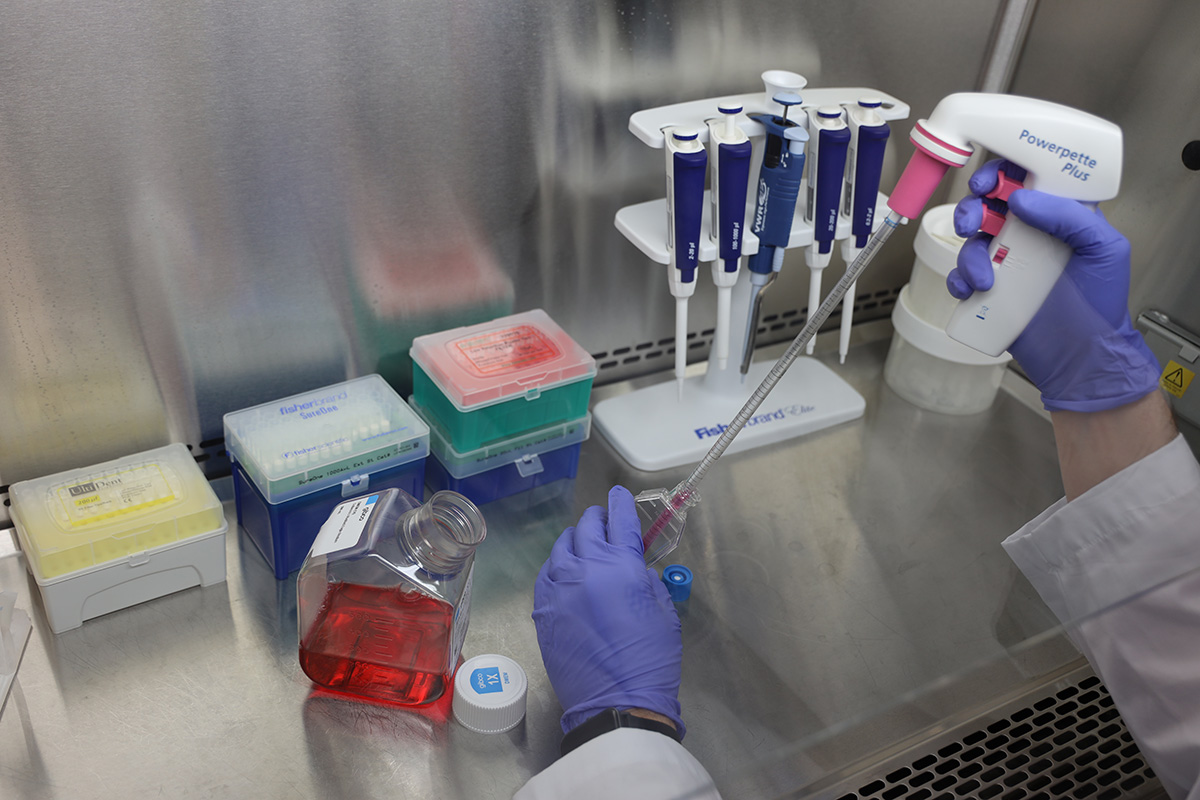
Launched in 2021, CTELab is supported by the Natural Sciences and Engineering Research Council to train and offers research opportunities to three graduate and three undergraduate students. The team is currently working on the Banting platelet project as well as research into how cells respond to their mechanical environment. One such project is conducted in collaboration with Carleton’s Impact Research Lab to observe how brain cells react to high-strain stretch that result in traumatic brain injury.
Harris and his lab team grow cells and tissues and uses super-resolution imaging techniques to characterize their properties. These tools include classic optical microscopy to visualize how a cell changes shape and interacts with other cells, as well as an atomic force microscope and a total internal reflection fluorescence microscope funded by a Canadian Foundation for Innovation grant.
The stabilization of blood bank supplies would have the biggest impact on patients with a chronic need for platelet transfusions. People with cancers or autoimmune diseases usually have very low platelet counts, sometimes close to zero. These patients are subject to easy cuts and bruises, blood that doesn’t clot and wounds that don’t heal. If enough platelets could be created in a lab, tailored to each patient’s needs, it could lead to personalized medicines that take the strain off the system and help the immunocompromised.
Further applications of Harris’s research could also include skin grafts and other tissue transplants. What need to come first is an understanding of how tissues behave and build themselves up at the cellular level.
“With that, I’m hoping my work can help figure out how to bioengineer the same mechanical properties of cells and tissues to use them in regenerative medicine.”
Friday, December 1, 2023 in Faculty of Engineering and Design, Health, Research
Share: Twitter, Facebook