By Tyrone Burke
Photos by Lindsay Ralph
When tissues in the human body are damaged, they repair themselves. It is how we heal, but it leaves scars behind.
With chronic inflammatory conditions like asthma, the scarring happens inside the body. The accumulation of connective tissue replacing normal tissues – parenchymal tissues, in scientific terminology – is called fibrosis. It can make symptoms worse or even cause fatal obstructions in the lungs.
“When you cut your arm, a little scar can develop. This happens because extra collagen is being produced and accumulating to close the wound,” says Leila Mostaço-Guidolin, an assistant professor of Systems and Computer Engineering who was awarded a Canada Research Chair (Tier II) in Imaging and Biomaterials Characterization.
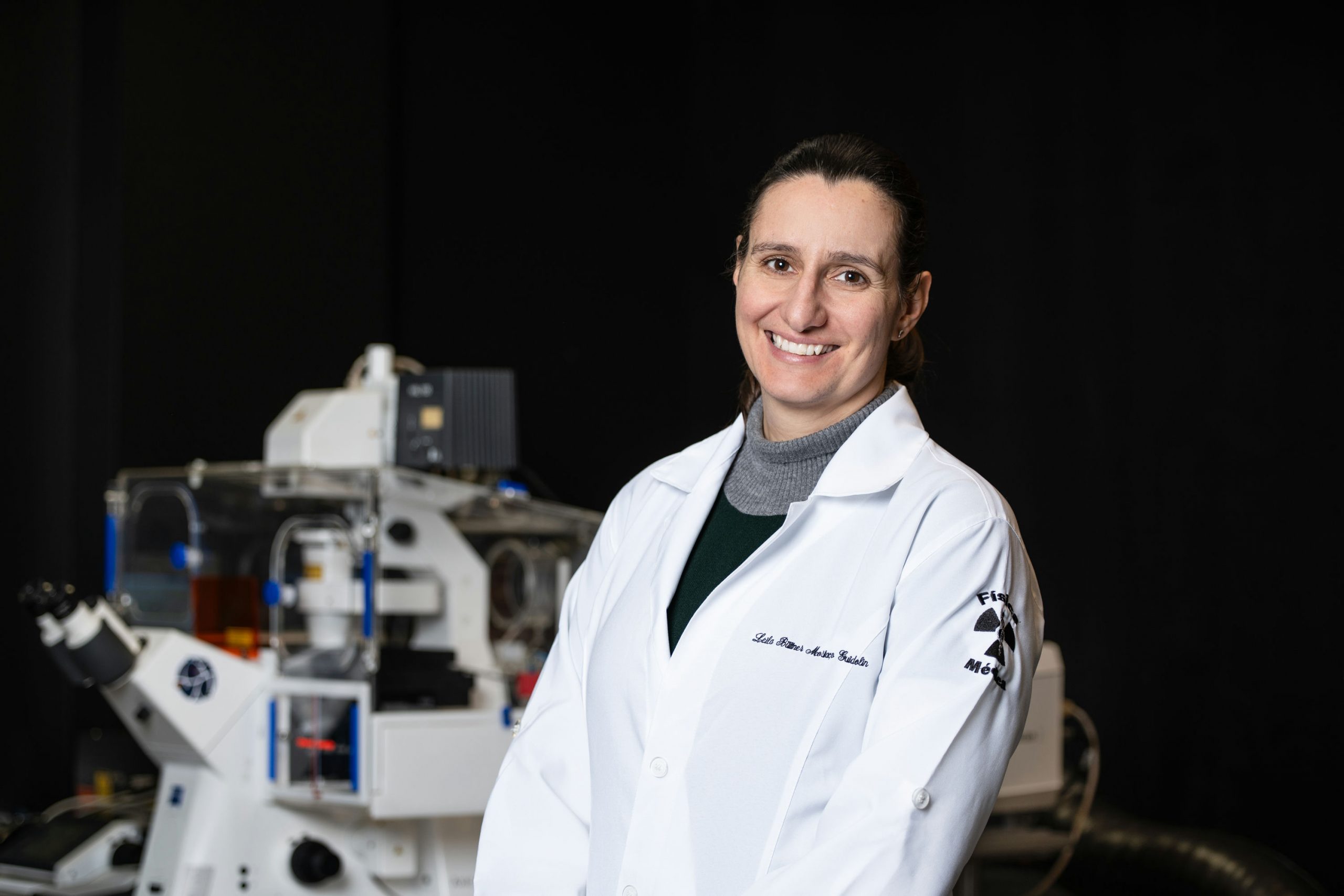
Leila Mostaço-Guidolin, assistant professor in Carleton University’s Department of Systems and Computer Engineering
“But quite often, the skin doesn’t move as it did before. The same thing can happen inside our body. When asthma is triggered by different factors like pollution, exercise or even cold air, it causes an injury in the epithelial layer of the lungs. Over time, that triggers a scar response.”
“One hallmark is that collagen builds up and, instead inflating and deflating normally, the lungs become more rigid and air does not pass through as it should. Nobody knows exactly what triggers this or how to reverse the changes.”
Understanding Fibrosis at the Cellular Level
Existing therapies like inhalers address the inflammation associated with fibrosis, but do not treat the fibrosis itself.
Mostaço-Guidolin is using advanced imaging technologies to better understand what is happening to the tissue structure, which could one day help develop treatments that address, or even reverse, fibrosis.
To do that, it will be necessary to understand more about what is occurring on a cellular level. Fibrosis changes the structure of lung tissue – and when a tissue’s structure changes, its ability to function properly changes too.
“We do not currently have a clear target for therapies,” says Mostaço-Guidolin.
“My main research combines imaging technologies and tissue engineering to better understand the fundamental mechanisms that cause tissue remodelling on the level of the tissue structure – what is happening and why things are happening the way that they are.”
A Route to Reversing Scar Tissue Damage
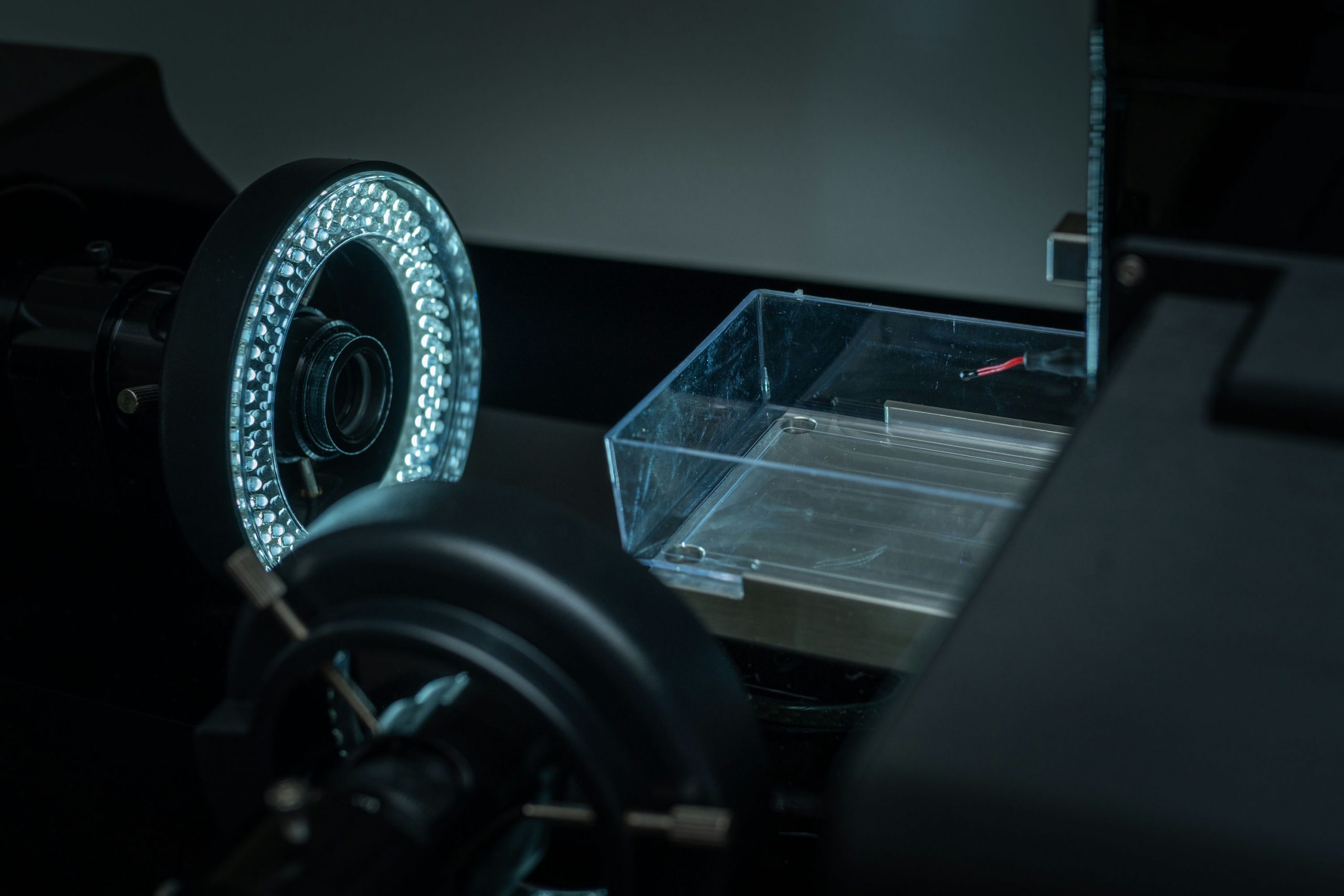
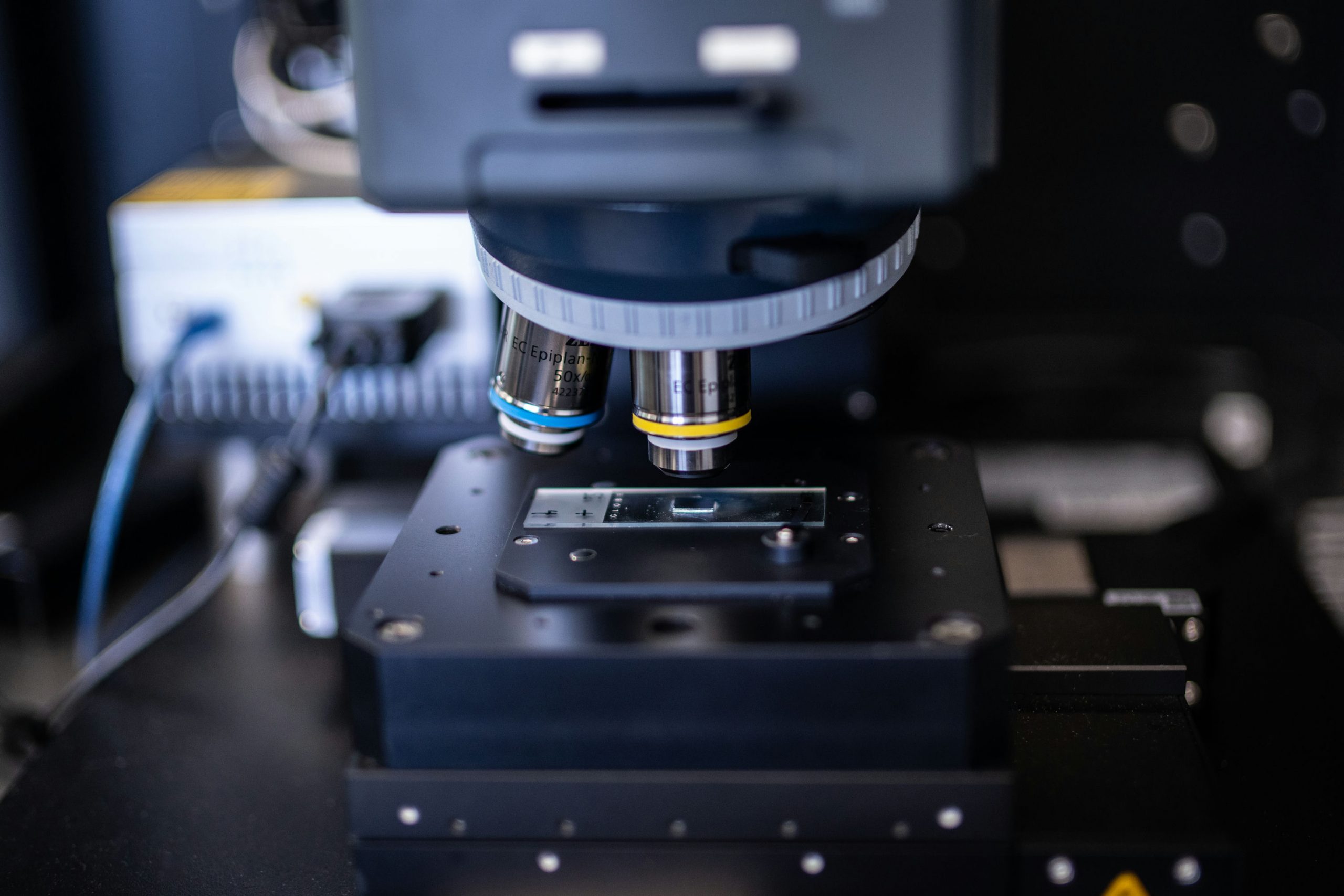
Mostaço-Guidolin uses nonlinear optical microscopy to study the structural details of collagen fibres, cataloging their characteristics. Using an imaging technique called second-harmonic generation combined with state-of-the-art detectors, she can examine the fibrotic tissue in a level of detail that was previously impossible. The tissue structure can then be characterized with a variety of metrics, one of them being entropy – a measure of the state of disorganization of the collagen fibres within the tissue.
“With fibrosis, the matrix structure of the tissue is more disorganized than normal. Imagine you have a bowl of noodles, and the noodles are very well placed in that bowl. That would be the normal structure of the tissue. But take the same bowl of noodles and chop them into little bits and pieces and throw them back in. The structure is going to be different. The cells there will not find a path from one place to another, just a lot of disconnected fragments. The microstructure they rely on to behave and function properly will be disrupted.”
That could be because fibroblast cells – the biggest contributors of forming connective tissues – are not making the collagen fibres properly. And collagen fibres being more fragmented might trigger more inflammation because our bodies perceive a need to repair the fragmentation – which could lead to more fibrotic tissue, which triggers more inflammation, and so on.

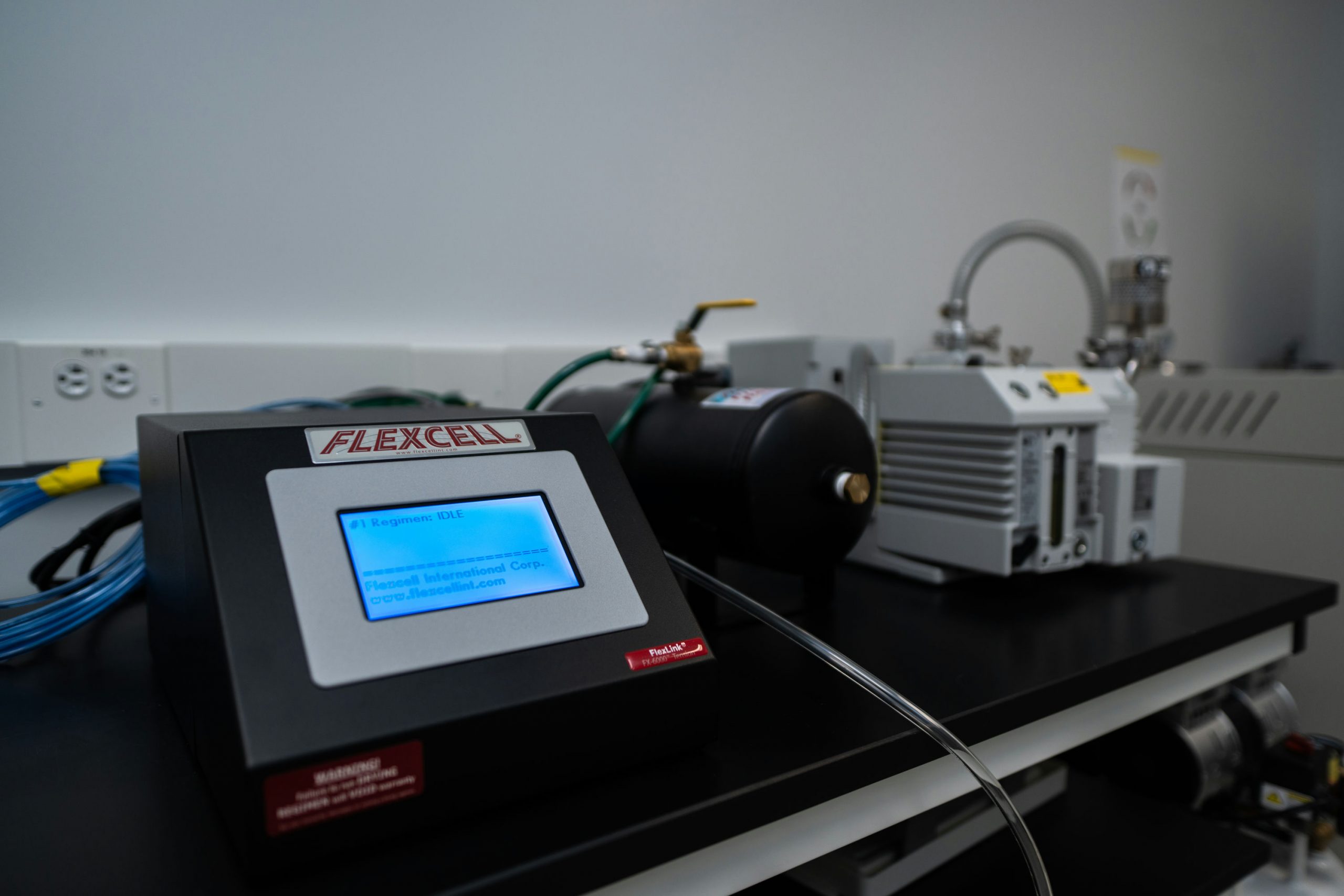
What is actually happening within these tissues remains an open question, but it is one that Mostaço-Guidolin hopes to answer. As part of her work as a Canada Research Chair, she also plans to use tissue engineering techniques to develop artificial tissue models and explore how drugs could affect cellular behaviour and whether it can be manipulated to reverse the tissue disorganization. Though her focus is primarily on asthma, this research could have broader implications for the treatment of many other diseases.
“If we can reverse the structural changes, we might be able to restore the function of the organs,” says Mostaço-Guidolin.
“I am focused on asthma and the lungs, but fibrosis can happen in any type of tissue. The fundamental mechanisms that cause it are an important piece of the puzzle. We need to understand these structural changes in order to control them.”