By Pat Armstrong, Hugh Armstrong, Jacqueline Choiniere, James Struthers and Ruth Lowndes
This article is republished from The Conversation under a Creative Commons licence. All photos provided by The Conversation from various sources.
There is no question that COVID-19 has had devastating consequences in long-term care for residents, staff and families. Media provided heart-wrenching stories about conditions in care homes and pictures of residents peering through windows. Numerous reports have been documenting the factors that contributed to the disaster, identifying once again what needs to change.
However, as is often the case in disasters, there are signs of light emerging from the devastation. Here we highlight three promising developments based on our current research project, “COVID-19, Families and Long-Term Care.”
Family councils
First, as we have learned through our interviews with family members, more people are participating in family councils and more family councils are becoming highly effective in shaping policies and practices.
A family council is composed of family and friends of a long-term care home’s residents. Although family councils are allowed in Ontario’s Long-Term Care Homes Act, the groups are intended to be self-led and democratically run, and determine their own goals. Within their overall purpose of improving quality of life for residents, their roles can include education, peer support and pursuing positive changes in homes and in the long-term care system. Whether there is a family council and how it operates varies with each home and is determined by it.
In Ontario, family councils are included in the legislation governing long-term care but are not required. Certainly, family councils have long played a critical role. But not all homes have had active councils and not all councils have taken the kind of action that pandemic practices have spurred.
During the pandemic:
-
Cut off from daily life in care homes and limited in the impact they could have individually, more family members joined the councils.
-
Frustrated by the poor communications from care homes, more councils became highly effective communicators.
-
Provoked by confusing government directives, councils more thoroughly investigated the directives in order to become critical sources of information for families and even sometimes for the management.
More councils have furthered their efforts both in relation to the home and in relation to government, connecting through family council networks and sharing information across jurisdictions to broaden their advocacy work. At the same time, the pandemic has made more people in the general population aware of conditions in long-term care and determined to demand change.
Essential contributions
Second, the prohibition against families entering care homes made their essential contributions visible. As we have long learned in our research, families — by which we often mean women — do much more than hug. They prepare culturally appropriate food and activities, purchase supplies and clean clothes and assist in eating and in walking. They monitor, advocate and interpret, and they brush teeth and comb hair — to name only some of the ways they fill the gaps in care.

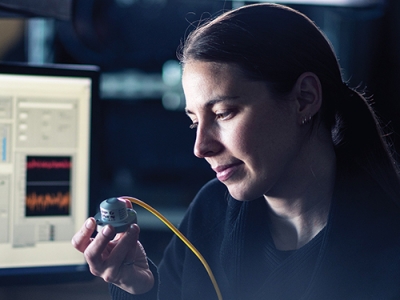
THE CANADIAN PRESS/Justin Tang
For example, one woman who visited her aunt said:
“I would wash her face. I would cut her hair, which she preferred I do rather than hiring somebody. And I would help her stay groomed. Her hands were often dirty, so I would soak her hands to get them cleaned up. I’d help her clean her dentures, brush her teeth, brush her mouth really. And I would help her with calling to family.”
She also cleaned her aunt’s wheelchair, and cleaned up anything she noticed that didn’t look good. She called staff’s attention to her aunt’s needs, such as her missing eyeglasses. And she would take her aunt outside.
“I would take her outside, which is a big thing for me because they’re not entitled to fresh air. I would take her outside as much as I could even if it was just a spin down to the sidewalk and back. And she loved actually being outside and smelling the air and seeing even the traffic go by. I mean, she didn’t care what it was. It was just like being part of life.”
With family visits prohibited, none of these aspects of care were provided for her aunt in the wake of COVID-19.
Although staff shortages were clearly critical during the pandemic, family absences exposed the extent to which chronic staff shortages before the pandemic have made homes dependent on relatives every day for a wide range of care.
Essential care
Third, the prohibition against visitors, combined with the enforced isolation of residents in their rooms and the push for staff to focus on clinical care, highlighted the essential nature of both social care and of those services often dismissed as supplementary. These include food, clothing, housekeeping and laundry.
After the Canadian Armed Forces deployed members to provide assistance in long-term care homes during the COVID-19 crisis, a report emphasized the absence of these essential services and the absence of vital social care. Specifically, it noted “not having witnessed any psychosocial support for these residents,” the lack of clean linen and lack of access to sufficient nutrition.

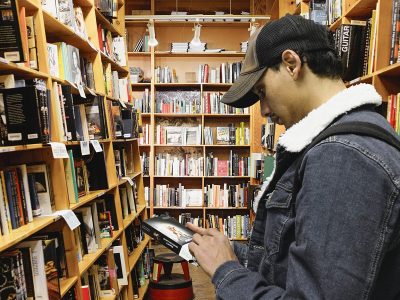
THE CANADIAN PRESS/Nathan Denette
The haunting pictures of residents in the windows and the reports of death from isolation also speak to a lack of social care. Clinical care is undoubtedly necessary, but COVID-19 makes it obvious it is not sufficient for life.
There is no question that we will have to work hard to make sure that this time the lessons learned from the pandemic do not get lost once again as the immediate crisis passes. This includes supporting families and family councils. It also means recognizing the full range of essential care.
![]()
Thursday, August 12, 2021 in The Conversation
Share: Twitter, Facebook