By Lisa Gregoire
Photos by Justin Tang
Mike Hildebrand fell asleep on the job once, in the parking lot of The Ottawa Hospital’s Civic Campus. It’s understandable, considering the demands of his research.
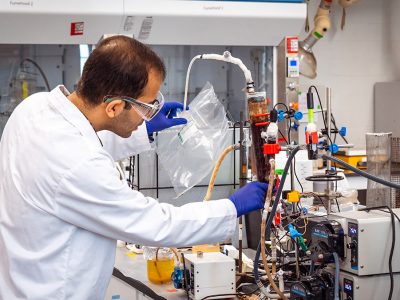
Hildebrand, a Neuroscience professor at Carleton, is trying to figure out, with the help of some graduate students, what’s happening in the spinal cord to perpetuate chronic pain, a scourge that impacts as many as one in five people, mostly older adults.
For nearly 10 years, Hildebrand used spinal cord tissue from rats to record electrical signals travelling between neurons and study the molecules, present or absent, that control the delivery of pain signals to the brain.

Like her Carleton collaborator Mike Hildebrand, Ottawa Hospital neurosurgeon and researcher Dr. Eve Tsai is focused on fixing devastating health disorders.
But thanks to a unique collaboration with Dr. Eve Tsai, a neurosurgeon and researcher at The Ottawa Hospital, Hildebrand’s team is now capturing recordings from spinal cord neuron synapses using human tissue, something they believe has never been done before.
“It’s so exciting, and I never really pictured it,” Hildebrand says about being the first in the world to attempt this experimental technique.
“I had more modest ambitions, I’d say, for my research. I thought, ‘I’ll have my niche and I’ll have a few students and we’ll answer some questions.’ It’s cool to see what new doors continue to open.”
The tissue that forms the basis of this groundbreaking research comes from human organ donors. Most research on human tissue, other than biopsies, involves potentially diseased tissue or takes place significantly after death. For neurons, that means the signalling pathways would be irreparably degraded.
“I wasn’t aware of research where you take viable healthy tissue,” says Hildebrand. “That’s what makes this so unique.”

On Duty After Dark
The fact that somebody has to die for them to conduct their work is not lost on Hildebrand and his students. They treat their work seriously: someone is on call 24 hours a day to respond to the hospital and receive the tissue in the event that an organ donor manifests.
But as with any hospital procedure, there can be delays, which is why Hildebrand was dozing in his car in the parking lot, waiting for word from the surgical team.
A father of three young children, Hildebrand confesses that was during the early days of this project; now it’s his students who are on duty after dark.
Dr. Eve Tsai (middle) with PhD student Annemarie Dedek and Neuroscience professor Mike Hildebrand.
On deck are master’s student Chaya Kandegedara and PhD student Annemarie Dedek. They receive the tissue in the operating room and then divide it up for Kandegedara’s biochemical experiments and Dedek’s electrical recordings. Her specialized recording setup measures currents from individual synapses between neurons and plots the results onto a squiggly graph.
“When I had it running for the first time at Carleton, I was calling colleagues over and saying, ‘Look at the screen!’ And it’s just a little blip,” says Hildebrand, describing his initial electrical recordings on rodent tissue with the verbal velocity and fervour of a child at a waterpark. “I’m always amazed. I never get bored of it.”
If Hildebrand and his students succeed in identifying what’s causing pain signals to keep firing, or what’s missing that usually blocks those signals, that could prompt pharmaceutical companies to develop drugs that could relieve people of debilitating daily pain.
Hildebrand thinks that’s worth pursuing, and he’s not alone. He and Tsai, in conjunction with two other labs, recently received a five- year $573,750 grant from the Canadian Institutes of Health Research to continue their work.

Pain Signalling
We have all felt pain. If you fall while skating on the frozen Rideau Canal and bang your knee, sensory impulses travel along neural pathways in your leg to your spinal cord, where they are first organized, and then new impulses relay that information to the brain.
The brain then analyzes the input and reacts, so that you “feel” pain and know that you’re injured. Pain signalling, which happens within a second or two, helps keep you alive by telling you something’s wrong.
But for some people, pain continues when it shouldn’t — long after a wound has healed, for instance, or a limb amputated — because of increased electrical impulses travelling to the brain or even impulses without sensory input.
Hildebrand believes we can understand pain better by studying the spine and chemically targeting damaged areas where signals are first organized and relayed. Although spinal pain signalling research has been underway for a couple decades, nobody is doing the same type of work — nor to the same extent — as he and his collaborators.
And while their project may offer tremendous hope for chronic pain sufferers, the truth is, Hildebrand might never have studied spinal cord neurons were it not for a stroke of bad luck.
“We have all felt pain”
Both Hildebrand and his wife Sara applied to teacher’s college after finishing undergraduate degrees in their hometown of Vancouver years ago. She got in; he did not. Disappointed and somewhat adrift, he took a year off to gain perspective and figure out what to do.
After some soul searching, he entered graduate school at the University of British Columbia and fell in love with scientific research — in particular, molecular and cellular neuroscience. His PhD supervisor Terry Snutch owned a small pharmaceutical company, so after graduating Hildebrand went to work for him, studying how chemical blockers affect the pain signalling of spinal neurons in rodents.
He then got a job as a research fellow at Sick Kids Hospital in Toronto, refining his research focus and mastering use of the electrophysiology recording equipment. Then, just shy of five years ago, he landed a position at Carleton that allowed him to continue his research and also teach and mentor students.
It was a dream job. Getting students excited about new material, showing them why it’s relevant, and seeing them meet their own challenges and excelling, is beyond rewarding, he says.
These days, Hildebrand teaches a third-year Neuroscience course and a fourth-year seminar. He also supervises five graduate students, including Dedek and Kandegedara, who are directly involved in the chronic pain research.

Bridging the Gap Between
Research and Clinical Trials
Tsai, Hildebrand’s main collaborator, also has two jobs rolled into one.
She is a neurosurgeon and researcher — an uncommon hybrid which involves performing brain and spinal cord surgeries at the hospital and also leading a lab at The Ottawa Hospital Research Institute. She and her lab colleagues are among the world’s leaders in efforts to repair and regenerate neurons in people with spinal cord injuries.
Tsai’s windowless office in the hospital’s Neuroscience Department is crowded floor-to-ceiling with stacks of paper, medical degrees, certificates of expertise, trophies and other awards, and precariously piled books such as Neurosurgery: Tricks of the Trade.
It’s a stark contrast to Hildebrand’s newly occupied office in Carleton’s Health Sciences Building, which was practically empty back in January, save for a jelly belly dispenser (his favourite treat) and a few family photos.
Tsai calls herself a translator — she understands the needs and challenges of both clinical neurosurgery and neuroscience research and can maximize outcomes on both sides.
Tsai, who got into the University of Toronto’s medical school at age 19 with only two years of undergraduate work completed, and then did her residency while she was earning a PhD, does research for one reason: to improve treatment for her patients. Which is probably why she and Hildebrand get along so well. Both want their lab work to focus on fixing devastating health disorders.
Hildebrand’s work identifying the mechanisms of pain processing in the spinal cord is particularly significant, says Tsai, because it helps to bridge the gap between research and clinical trials. Most pharmaceutical clinical trials occur after a long period of research, usually on animal tissue. But what works in animals doesn’t always work for humans.
Clinical Trials for Chronic Pain Therapies
Hildebrand, who’s now proving that at least some results from animal testing are applicable to humans, is helping to accelerate progress toward clinical trials for chronic pain therapies, Tsai says, and also helping to inform her own research into the human spinal cord and related research around the world.
Hildebrand has lab space at The Ottawa Hospital, thanks to Tsai’s support, so their teams can co-ordinate receipt of donor tissue and share space and data. Tsai and Hildebrand also meet regularly to talk about their work, she says, to their mutual benefit.
“Now that we have gotten them this tissue, they are able to work out techniques that really have not been developed well because the reality is, we have not had access to this tissue before. So now we can start to study things that we have not really studied before, and see whether we can apply them to patients,” says Tsai, praising Hildebrand for his drive and enthusiasm.
“You cannot really succeed as an individual. You have to have all the stars align around you.”
That’s another area where Hildebrand and Tsai agree.
“A lot of what we’re doing is built on the foundational work of lots of others,” he says. “Canada is a world leader in pain research. A lot of the biggest names in pain research are Canadian. I’m really blessed at having come from that training and exposure.”

Monday, July 9, 2018 in Faculty of Science, Health, Research
Share: Twitter, Facebook